Gene Therapy Breakthrough Offers Hope for Huntington’s Disease
A New Dawn in Neurogenetic Medicine
In a medical first, scientists have achieved a successful gene therapy trial that slows the progression of Huntington’s disease, marking a watershed moment for genetic medicine. This inherited brain disorder — long seen as a relentless death sentence — might finally be confronted with a treatment that modifies the disease’s root cause rather than merely alleviating symptoms.
Huntington’s disease (HD) is caused by a mutation in the HTT gene, which produces a toxic form of the huntingtin protein. This defective protein accumulates in neurons, leading to progressive brain degeneration that destroys movement control, cognitive function, and mental stability. Until now, treatment options were limited to managing symptoms with drugs that offered only temporary relief.
The new gene therapy, developed through a multi-institutional collaboration involving European and North American research teams, represents a paradigm shift — not just in HD treatment, but in how we approach inherited neurological diseases as a whole.
The Science Behind the Breakthrough
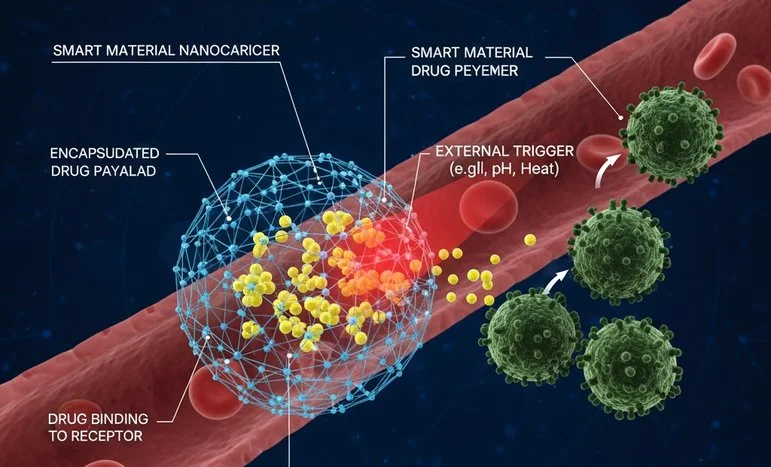
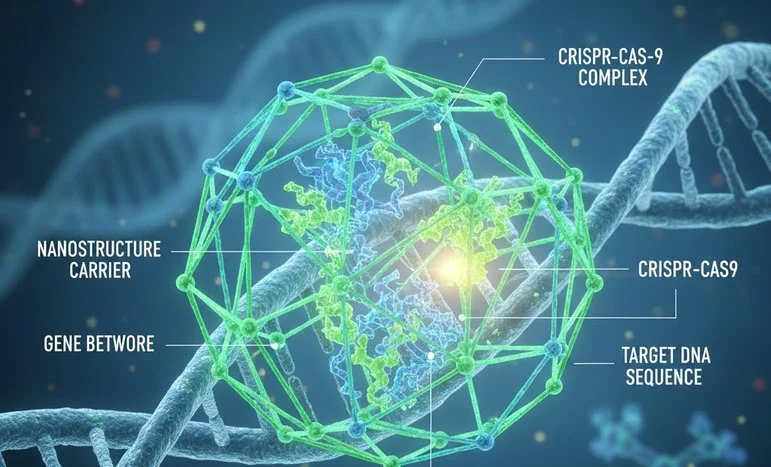
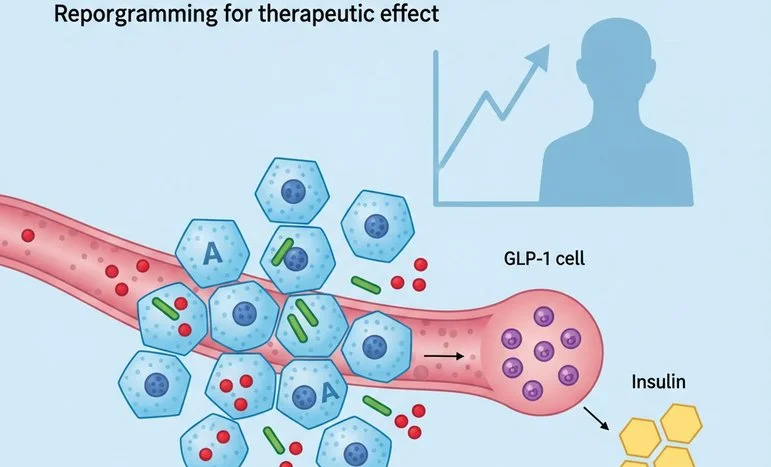
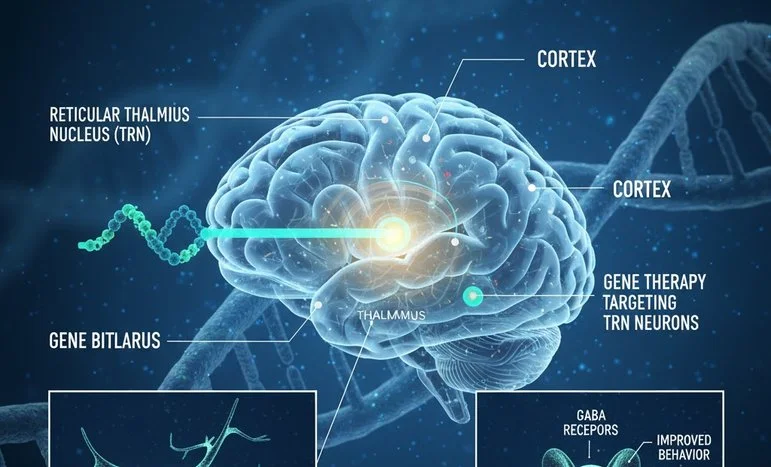
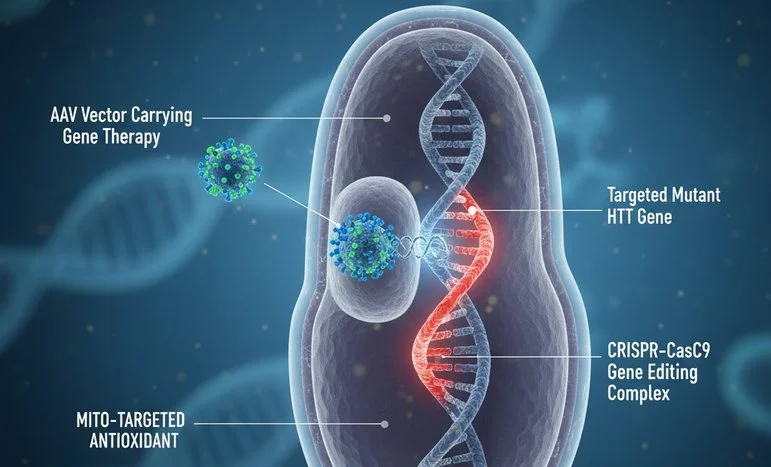
The gene therapy trial used a technique called allele-selective silencing, a clever genetic strategy that targets only the mutant copy of the HTT gene while preserving the healthy version. This precision prevents unwanted side effects and maintains normal cellular function — a key improvement over earlier approaches that indiscriminately shut down both gene copies.
Using an engineered viral vector (commonly derived from adeno-associated viruses, or AAVs), scientists delivered the therapeutic genetic material directly into specific brain regions most affected by HD, such as the striatum and cortex. Once inside, the therapy reduces the production of the harmful mutant protein, allowing neurons to function longer and delaying disease progression.
Early trial results show measurable improvements in motor coordination, cognitive function, and overall neural stability. MRI scans revealed slower brain atrophy rates, while biochemical tests confirmed reduced levels of mutant huntingtin in cerebrospinal fluid — a biological marker of treatment efficacy.
A Turning Point for Families Living with Huntington’s
For decades, families affected by Huntington’s disease have endured an emotional roller coaster. Because it is an autosomal dominant disorder, each child of an affected parent faces a 50% chance of inheriting the condition. Genetic testing can confirm the presence of the faulty gene long before symptoms appear — but until now, knowing one’s status offered no path to prevention or cure.
With this breakthrough, the narrative changes dramatically. For the first time, early detection could lead to early intervention, transforming HD from an inevitable decline into a manageable condition. Patients who once viewed genetic testing as a sentence of despair might soon see it as a gateway to timely treatment and extended quality of life.
Families involved in the trial have reported not only clinical improvements but also psychological relief — the sense that modern science is finally catching up to a disease that has haunted their bloodlines for generations.
Challenges on the Road Ahead
Despite the promising results, experts caution that the path to broad clinical use remains challenging. The current trial involved a small cohort, and while it achieved safety and efficacy milestones, larger phase III studies are required to confirm long-term benefits and detect rare side effects.
Gene therapy’s success depends heavily on delivery accuracy, dose optimization, and immune response management. The brain’s delicate environment poses unique challenges — immune reactions, inflammation, or off-target effects could undermine safety. Furthermore, the cost of producing and delivering AAV-based therapies remains prohibitively high, raising concerns about global accessibility.
Another critical aspect is duration of effect. It is unclear whether the therapeutic gene silencing will last for decades or whether patients may require repeated interventions. Scientists are already exploring next-generation vectors and CRISPR-based refinements to achieve more permanent, controllable results.
Ethical and Social Implications
As with all gene-based interventions, the ethical dimensions of this achievement cannot be ignored. Huntington’s disease sits at the intersection of genetics, family inheritance, and identity. Many individuals with a family history of HD avoid genetic testing to escape the emotional burden of a positive result. Now, with gene therapy showing promise, this hesitation could shift — but it also raises questions about genetic privacy and discrimination.
Insurers, employers, and even governments could misuse genetic data if proper safeguards aren’t enforced. Furthermore, society must confront how to manage reproductive choices in the age of curable genetic disorders. Will gene therapy lead to genetic selection pressures or new forms of inequality based on access to advanced medicine?
Thus, while this success deserves celebration, it also calls for ethical vigilance to ensure innovation serves humanity rather than divides it.
The Ripple Effect: Beyond Huntington’s Disease
This therapy’s significance extends far beyond Huntington’s alone. The success of an allele-selective genetic intervention sets the stage for treating other dominant genetic disorders — from ALS (Amyotrophic Lateral Sclerosis) to certain forms of Alzheimer’s and Parkinson’s diseases. The same principles of targeted silencing and viral delivery can be tailored to countless neurodegenerative conditions once deemed untreatable.
Moreover, this trial reinforces the promise of personalized medicine — an approach where treatments are designed based on each patient’s unique genetic profile. As sequencing costs drop and biomanufacturing scales up, we are approaching a future where genetic correction becomes a standard therapeutic option rather than a scientific novelty.
The Global Health Perspective
From a public health standpoint, the Huntington’s gene therapy success symbolizes the dawn of precision healthcare equity — but only if the technology reaches beyond wealthy nations. Huntington’s is not confined to one demographic; cases exist across Europe, the Americas, India, and Asia. Ensuring affordable global access to gene therapy will determine whether this discovery remains a milestone for science or a privilege for the few.
Organizations like the World Health Organization (WHO) and global gene therapy consortia must play an active role in developing fair-pricing models, technology-sharing frameworks, and regional gene manufacturing hubs. Equitable access must be embedded in innovation from the start — not as an afterthought once profits have been secured.
A Glimpse into the Future of Neurological Care
Looking ahead, gene therapy for Huntington’s could become part of a multi-modal treatment framework, combining genetic correction with neuroprotective drugs, AI-based disease monitoring, and rehabilitative robotics. Machine learning algorithms could analyze brain imaging and genetic data to tailor therapy schedules, while wearable devices track subtle changes in motor or cognitive performance.
In the longer term, stem cell regeneration and brain-computer interfaces might complement genetic therapies, offering a holistic approach to restoring lost function. Such integration could make neurological care not only curative but adaptive and personalized in ways unimaginable a decade ago.
Conclusion: From Despair to Determination
The first successful gene therapy trial for Huntington’s disease marks a moment of hope born from decades of perseverance. For families who have watched generation after generation succumb to the same genetic fate, this breakthrough signals the beginning of a new story — one written in the language of science, compassion, and courage.
It reminds us that the essence of medicine lies not just in curing disease but in restoring dignity and possibility to those once forgotten by fate. As researchers move toward larger trials and eventual approval, the world watches with optimism — knowing that each step forward for Huntington’s disease is a step forward for humanity itself.
🧬 Final Reflection
The Huntington’s gene therapy success is not just a scientific achievement — it’s a moral one. It shows what happens when human intellect and empathy converge. As we decode the genome’s darkest mysteries, let us remember that every code we rewrite must honor the very thing that makes us human: our shared hope to heal.
We appreciate that not everyone can afford to pay for Views right now. That’s why we choose to keep our journalism open for everyone. If this is you, please continue to read for free.
But if you can, can we count on your support at this perilous time? Here are three good reasons to make the choice to fund us today.
1. Our quality, investigative journalism is a scrutinising force.
2. We are independent and have no billionaire owner controlling what we do, so your money directly powers our reporting.
3. It doesn’t cost much, and takes less time than it took to read this message.
Choose to support open, independent journalism on a monthly basis. Thank you.